Welcome
Whether you're experiencing breastfeeding grief, supporting someone through it, or simply want to know more, I hope this page helps.
Breastfeeding grief, loss, or trauma exists. It matters and it’s real. You might feel many different emotions and no two experiences are exactly the same. It doesn’t mean you aren’t grateful that your baby is being fed. It doesn’t mean that you prioritise your own feelings over your baby’s needs. It is possible to feel many emotions at the same time.
Breastfeeding grief can be caused by many things. Maybe you had to stop before you were ready. Maybe you had a really difficult experience that looked nothing like you hoped. Maybe you weren’t given the support you needed, or others tried to damage your experience. Most likely you were trying to breastfeed in a system that told you it was great but then didn’t provide you with an environment that actually made that possible.
On this page you’ll find a collection of everything I have written over the years about breastfeeding grief, loss and trauma including my social media posts, articles and interviews. There are ideas for what might help, where to find more support and further reading.
My work is based on twenty years of research exploring experiences of infant feeding, and particularly how this can affect mental health and wellbeing. Specifically my breastfeeding grief research stems from a large study of over 3000 women who struggled with their breastfeeding experiences. I hope some of it resonates with your experience.
My book 'Why breastfeeding grief and trauma matters' is available from my website, via Amazon / Wordery / most bookshops and there is an Audible and Kindle version.
WHAT CAN BREASTFEEDING GRIEF FEEL LIKE?
-c6becb8.png/:/rs=w:370,cg:true,m)
-0a64eaf.png/:/rs=w:370,cg:true,m)
-ce47326.png/:/rs=w:370,cg:true,m)
-593e1f8.png/:/rs=w:370,cg:true,m)
-f9176b3.png/:/rs=w:370,cg:true,m)
-eb75657.png/:/rs=w:370,cg:true,m)
-79ae241.png/:/rs=w:370,cg:true,m)
-d7d01ae.png/:/rs=w:370,cg:true,m)
GRIEF IS A NORMAL REACTION TO LOSS

Grieving the loss of a breastfeeding relationship, no matter how long or short, is a completely normal & understandable reaction. But we’re often not very good at dealing with difficult emotions are we? People feel awkward. They want to play your emotions down. Or they may simply dismiss the idea that things bothered you in the first place.
This seems to be especially true of grief attached to being a woman. Women’s bodies and emotions are just a bit too complicated and messy for our society. And that’s before we even get started on the discomfort we feel when women are angry, especially when it is anger directed at the patriarchal system that causes the things that make us angry.
Grief is an utterly normal reaction to loss, and we should probably all spend more time grieving when we lose things that are important to us rather than trying to push those emotions away. And many women do, at least in hindsight, identify those feelings when they can’t breastfeed as grief and loss.
As a society we should recognise this grief for what it is, and support & encourage women to be able to grieve that loss. As humans, sadness is something we need to feel & process, and it is a normal response to negative things happening in our lives.
This is not to say it isn’t completely awful when you’re in the depths of it, but it does show you are having a healthy reaction to a negative thing.
A big problem with breastfeeding grief though is rather than seeing it and supporting you, people can react badly. Very badly.
- They try and tell you it doesn’t matter (‘the main thing is your baby is fed’)
- Or make out it isn’t real grief or serious enough (‘but you have a healthy baby’)
- Or that it doesn’t matter now (‘Why worry - he’ll go off to uni & live off beer & pasta’)
- Or simply ignore it altogether.
Feeling dismissed intensifies grief or sends you to a place where you can’t process it and move forward. Yet again, we just need to listen to women. If she tells you it matters, it matters.
IT'S NOT ALWAYS JUST ABOUT THE MILK

The UK & Ireland have the lowest breastfeeding rates in the world. This isn’t to be mixed up with intention; we often really want to breastfeed. But our hopes and dreams for feeding and caring for our baby in a certain way get rapidly dashed.
During pregnancy we're urged to breastfeed and told ‘breast is best’ (I hate that useless phrase) but after the birth we find that support, possibly from the health service, family, workplaces and society in general just isn’t there or is actively working against our intention. We end up with complications, confused about what to do, or simply finding it all too much, and end up stopping, often before we are ready.
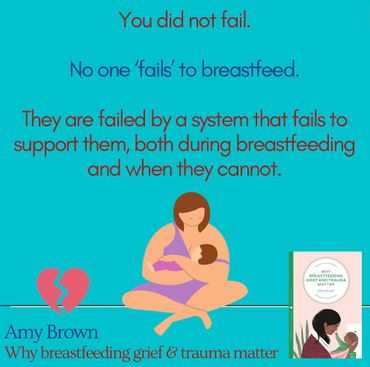
And when we do? We blame ourselves. ‘I couldn’t breastfeed’ or ‘I should have tried harder’ or ‘I failed’. Nonsense. Every woman I have ever spoken to who stopped before she was ready tells me a story where someone could have done something, or something could have been different. But instead, our society deflects responsibility and leaves women blaming and even hating themselves for their decision.
These feelings can last a long time. The oldest ‘baby’ a mother ever told me about, explaining that she was not able to breastfeed, had just retired. He was off playing golf and his mother, in her late 80s, was still grieving not being able to feed him how she wanted.
It’s not just about the milk. Yes on a population level breastfeeding protects maternal & infant health, but that’s not the only reason why many feel terrible when they stop.
We might be fine with giving our baby formula. Grateful. But it’s so much more complicated than that. We are affected by our experiences of trying to feed. Pain and exhaustion. Not being supported by others. Wanting to use our body in a way we were told would work and it not playing ball. Our preferred way of caring for our baby vanishing. Spiritual, religious or cultural ties being severed.
Breastfeeding has always been so much more than simply providing milk to a baby, yet we act as if every breastfeeding problem is simply fixed by giving formula.
When we talk about breastfeeding trauma, what do we mean?

The concept of trauma, or post-traumatic stress disorder (PTSD), was first described in response to symptoms soldiers suffered on coming home from war. They had nightmares and flashbacks, startled easily and experienced a whole range of emotions including anger, sadness and self-blame.
Subsequently, clinical criteria were put in place to diagnose conditions like PTSD. These criteria typically focused on a serious, life-threatening event being central to any trauma experience.
Now some women may experience a life threatening event for them or their baby. Perhaps they had serious complications in labour. Perhaps their baby was in neonatal care. Perhaps their baby lost a lot of weight. Or maybe they experienced extremely painful nipple trauma or infection.
But many psychologists and therapists think more widely than that. There is increasing recognition that perhaps we should spend less time focussing on what happened when determining whether someone is traumatised and instead look at their symptoms and how they feel. Trauma can mean different things to different people.
Here are some broader definitions of trauma. Do you think they are a fitting description of how some women feel about their breastfeeding experience?
"Individual trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life-threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being". (Centre for Mental Health)
"The individual’s ability to integrate his/her emotional experience is overwhelmed". (NHS)
"Psychologically, the bottom line of trauma is overwhelming emotion and a feeling of utter helplessness". (Substance Abuse and Mental Health Services Administration)
This is not to say that everyone who has experienced breastfeeding difficulties is traumatised. As above, grief is a normal reaction to loss and there is a whole spectrum of different emotions you might feel. It's absolutely normal to be upset and angry after a difficult experience.
But sometimes these feelings don't go away, start to cause us a lot of distress and may interfere with the rest of our lives. Here are some signs that might suggest seeking more support might be helpful:
-71b1467.png/:/rs=w:370,cg:true,m)
-74850ac.png/:/rs=w:370,cg:true,m)
-969d511.png/:/rs=w:370,cg:true,m)
-02bddd1.png/:/rs=w:370,cg:true,m)
-66ea82d.png/:/rs=w:370,cg:true,m)

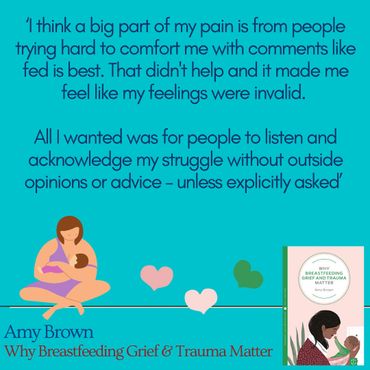
WHAT ABOUT SAYING 'FED IS BEST?'
.png/:/rs=w:370,cg:true,m)
.png/:/rs=w:370,cg:true,m)
.png/:/rs=w:370,cg:true,m)
.png/:/rs=w:370,cg:true,m)
.png/:/rs=w:370,cg:true,m)
.png/:/rs=w:370,cg:true,m)
.png/:/cr=t:0%25,l:0%25,w:100%25,h:100%25/rs=w:370,cg:true)
.png/:/rs=w:370,cg:true,m)
.png/:/cr=t:0%25,l:0%25,w:100%25,h:100%25/rs=w:370,cg:true)
WHAT WE MEAN WHEN WE CALL FOR 'MORE SUPPORT'

"The phrase ‘we need better support for breastfeeding’ can sometimes feel like a suggestion that if women just had a little more help latching their baby on, and tried a little harder, then all their problems would disappear. It can attract a lot of backlash, and with that perception you can understand why.
But when we call for ‘more support’ we don’t mean that at all.
Yes, support for breastfeeding can mean someone to sit and help you latch your baby on, moving them a little left or right so that latch is more effective and comfortable for you. And timely, skilled support like this can make all the difference to breastfeeding working out.
But it’s certainly not the only thing we mean. We mean that women deserve high quality information about how to know when breastfeeding is working... and when it isn’t. A better environment to breastfeed in. Acceptance. Value in what they are doing. Investment in the infrastructure that makes it that bit easier. And more than that again.
Most of these things are nothing to do with mothers directly at all but rather the people and systems around them who could do more to give her the best possible chance to breastfeed. Things like
- Ensuring there are specialists available, and quickly
- Investment in more staff and services
- Referral pathways for complications
- Enhanced training for all professionals who could influence feeding
- Proper support when breastfeeding is not possible
- Better workplace and employment protection
‘More support’ doesn’t suggest that with a bit of help and determination that all women can breastfeed. Rather it highlights how women are currently being let down at every level. The list is long, and likely incomplete. We have far to go but while women are still falling through the gaps at every stage we will keep fighting for ‘more support’ across every dimension this entails.
Healing from breastfeeding grief

There are several things that might help if you are struggling with your breastfeeding experience or how it ended. Each of these might be right for different people in different circumstances. There will be no one right way for everyone.
The first idea is to let yourself recognise that how you are feeling is normal. If you’re grieving breastfeeding I bet that you have people telling you it just doesn’t matter, or not even pausing to consider that it might. We know that most mean well. When people tell you that the main thing is that your baby is fed, they either don’t realise how important breastfeeding was to you, or genuinely think it will help. Some may be comforted by these words, but for others it can make things worse.
With other losses, such as the death of a loved one, people recognise the importance of loss and rituals as part of the grieving process. Yet with breastfeeding grief, you’re often just expected to get on with things.
It’s important that you recognise your emotions and give yourself time to grieve. Miriam Labbok spoke about the importance of treating this grief like any other grief and taking time to work through the different emotions.
Theories of grief acknowledge that everyone’s response to a loss is different, with people feeling and responding differently. There is no one right way to feel or one right way to act.
Models that look at grief often talk about 5 stages, but in reality these describe 5 different things grieving people go through, rather a set order. These include denial, anger (at yourself or others), bargaining (could I have done something differently?), depression and finally, hopefully, some kind of acceptance.
So take time to recognise how you feel, know that it is justified & normal and that over time, your feelings will likely change - though they won’t necessarily go away. For some, this may be as you move out of the baby stage and there is less focus on breastfeeding, so if you are still in those early days, know that this is a possibility.

It is so easy to blame ourselves when things go wrong. We think that if only had we tried a little harder or done something else then things might be different.
Firstly, it’s easy to think like this with the benefit of hindsight, and secondly, we know that when a woman cannot breastfeed, her experience is rarely straightforward.
If you’re blaming yourself, ask – did I really get all the professional support I needed, including medical testing and diagnosis if things weren’t working physically? Did my family really support me? Did my partner really do everything they could to help? Was I supported and valued as a mother trying to breastfeed her baby? What information and advice was I given from people who I trusted?
In the vast majority of cases women have been let down at least on one of these points. We do not live in a society that values, accepts and protects breastfeeding mothers. We set them up to fail – subtly and more directly – by placing numerous barriers in their way.
Never ever feel that you have not done the ‘best’ for your baby. You have – it is just that what is best for your baby and family turned out to be different from what you’d hoped.
When breastfeeding doesn’t work for physiological reasons it is no more your fault than it is if your eyesight isn’t perfect, but there are tests for that and we all accept not everyone has 20-20 vision.
In her book on birth trauma, Dr Emma Svanberg talks about an exercise called ‘the perfect nurturer’. In this exercise she asks you to think about the kindest, warmest, most caring person that you either know or can imagine.
Then, whenever you find yourself feeling ashamed or guilty, ask yourself – what would they say? Would they go ‘Oh yeah, actually Betty, you’re sooo crap,’ or would they kindly point out everything you had tried to do and how you were now caring for your baby?
Finally, know that you are not alone in this. So many women are being let down. It’s not just you. It’s a systemic issue that is bringing many women to their knees. Blame the system, not yourself.

Talking about how you feel can be very cathartic. This might be as simple as opening up to a friend who you know will understand, or you might prefer to reach out to someone who is professionally trained in counselling.
It might be telling friends and family that this matters to you and why. It might be speaking out in a more public way, sharing your experiences and emotions. It might be blogging, privately or anonymously.
It is worth thinking about who you talk to. If breastfeeding was important to you, you might want to be cautious about sharing how you feel with anyone or any organisation that you think might give a ‘the main thing is your baby is fed’ message.
Remember that breastfeeding support organisations are not just there when you are breastfeeding. An important part of their work is to support women who have not been able to breastfeed for as long as they wanted. They can help you by talking through how you feel, and helping you work through what may have led you to this point – emphasising the point that breastfeeding is affected by so many things and it is not your fault that your breastfeeding experience was so challenging.
Some of the main organisations in the UK include:
National Breastfeeding Helpline: 0300 100 0212
ABM: 0300 330 5453
La Leche League: 0345 120 2918
National Childbirth Trust (NCT): 0300 330 0700
You may also find that your local breastfeeding or parenting support group can offer support.
Alternatively, you might want to work with a lactation consultant, particularly if you had a breastfeeding complication that led to you stopping. Again, they would be very well placed to help you explore what happened to you and how you are now feeling. They are not only there to make breastfeeding work, but take a holistic approach to infant feeding as a whole. They can also support you with any queries you have about bottle- feeding and formula.
You can find a local lactation consultant on the Lactation Consultants Great Britain website - although many will now also give online support meaning location is less of a barrier https://lcgb.org/find-an-ibclc/
Another option might be to talk to a doula. You might think doulas are focussed on supporting women through birth, but postnatal support and debriefing is a key part of their role.
There are also a number of specialist midwives, health visitors and other birth and parenting experts who are now providing specific listening and counselling options for those experiencing breastfeeding grief. I recommend searching the www.bacp.co.uk website for specific perinatal counsellors.
One specialist perinatal trauma counsellor who I can personally vouch for is Kath Harbisher at the Bent not Broken project https://www.bentnotbrokenproject.co.uk . Alongside her qualifications Kath has many years experience of working as a doula.
Finally, another book I recommend for some practical exercises in exploring your grief is 'Healing Breastfeeding Grief: How mothers feel and heal when breastfeeding does not go as hoped' by Hilary Jacobsen.

One of the core approaches to helping people who are experiencing grief is not only to explore the roots of how they feel, but also to help them cope with any symptoms they are experiencing.
Everyone is different - and has different needs and barriers in terms of time, resources & physical ability - but here are some ideas to try, adapting them to what works for you:
Give yourself permission to look after you. To take time for yourself. To prioritise you.
Get outside. Nature is restorative if you are experiencing anxiety and feeling on edge
Be active. Exercise can help burn off adrenaline & release feel-good endorphins. Try and focus on your body as you move – feel the movement, your heart rate & notice your surroundings. Or scream into the forest / take up boxing.
Try not to shut yourself off from everyone. Choose your friends carefully, but don’t isolate yourself. Talk about how you feel to someone who will listen.
Don't be afraid to ask for professional support. Explore counselling, support from a breastfeeding organisation, or holistic support from a doula. See yesterdays post.
Share your experience more publicly with others. Blog. Record something for social media. Or write more privately to get your own thoughts out of your head.
For some volunteering can help both in taking your mind off things and doing something that will make a difference to others in the future. Perhaps support one of the breastfeeding or trauma organisations. Or try something completely different and new.
Try to calm your system. Relaxation exercises such as breathing and noticing things around you can help calm you down. Comfort yourself. Do you have a favourite smell, taste, place, piece of music or clothing that helps relax you? Might yoga or meditation help you?
For some people, keeping a diary and writing down their thoughts helps. For others, relaxing tasks that keep your mind distracted are useful – jigsaws, colouring, knitting etc.
Challenge your negative thoughts. Are they really true? Imagine a friend was telling you the same things. What would you say to them?
Try to look after your health. You know the drill. Plenty of sleep, a balanced diet, watch the alcohol.

If you are in the depths of grief, this may not be an option that is right for you at the moment. But as you move forward, you might want to think about how your experiences could be used to better support women in the future.
Your hospital should have its own Patient Advice and Liaison Service (PALS) or Maternity Voices Partnership (MVP), which you can use to feedback and/or complain about care received.

Sadly, if you haven’t been able to breastfeed as long as you wanted and you are grieving, you are one of a club that is growing every day.
So many women are being let down. It’s not just you. It might feel like everyone around you is telling you it doesn't matter, but many, many women feel the way that you do. It is not unusual. You are not over reacting. It did matter.
It’s a systemic issue that is bringing many women to their knees. Blame the system, not yourself.
You did not fail. Your experience does matter. You are allowed to care about more than whether your baby is fed.
Let's make things better for the future.

On the subject of making things better for the future, I'm often asked 'what can I do?' Here are some ideas. Remember there is never such a thing as making too small a difference - helping one woman or family can have a ripple effect across communities.
- Write to your local MP and ask them what they are doing to support infant feeding
- Support local and national breastfeeding and parenting charities, either with donations of money, time or amplifying their work
- Share evidence based infant feeding information on social media
- Support friends, family and others in your community who have new babies with evidence based resources and sources of support
- Talk about your story to others - help them to know that these emotions can be normal and are not a criticism of others
- You might even want to consider training with one of the breastfeeding organisations yourself to support more women and families in the future. You might be surprised to know that many of today’s peer supporters, breastfeeding counsellors and lactation specialists are not in their roles purely because they had an easy, fabulous time breastfeeding – but in fact because they experienced the exact opposite. Many had difficult experiences and stopped breastfeeding before they were ready, or needed to use formula when they didn’t want to. They get it. They’ve been there. They understand.
READ MORE...
Breastfeeding loss... or theft?
ABM magazine: Supporting mothers who haven't been able to meet their breastfeeding goals
Glamour Mag: Why we need to talk about breastfeeding grief
We may feel loss. We may be starkly aware of what is missing. But did we lose it? Did we do something to misplace it or prevent it? Absolutely not. It was stolen from us.
Glamour Mag: Why we need to talk about breastfeeding grief
ABM magazine: Supporting mothers who haven't been able to meet their breastfeeding goals
Glamour Mag: Why we need to talk about breastfeeding grief
‘A fundamental mothering experience had been snatched from me’: Why we need to talk about breastfeeding grief' in Glamour Mag
ABM magazine: Supporting mothers who haven't been able to meet their breastfeeding goals
ABM magazine: Supporting mothers who haven't been able to meet their breastfeeding goals
ABM magazine: Supporting mothers who haven't been able to meet their breastfeeding goals
The importance of supporting women who haven’t
been able to meet their breastfeeding goals
My Baba - is fed best?
Welldoing: Why breastfeeding grief and trauma matter
Welldoing: Why breastfeeding grief and trauma matter
We deserve more than our babies simply being fed. We deserve investment and value whatever approach we decide is best for our families – and importantly support, answers and recognition if our body isn’t working and we can’t feed our baby in the way we wanted.
Welldoing: Why breastfeeding grief and trauma matter
Welldoing: Why breastfeeding grief and trauma matter
Welldoing: Why breastfeeding grief and trauma matter
We need to talk more openly about why breastfeeding is more than just a milk delivery system for many women, in a way that doesn’t feel like a criticism to those who make different decisions. Women’s desires matter. Their bodies matter. Women matter, full stop.
Breastfeeding is good for mothers’ mental health – but those who struggle need support
Breastfeeding is good for mothers’ mental health – but those who struggle need support
Breastfeeding is good for mothers’ mental health – but those who struggle need support
Mothers who cannot breastfeed are absolutely not failing, rather, they are being failed – by a government who is far too quick to promote breastfeeding without protecting it.
Traumatic breastfeeding experiences are the reason we must continue to promote it
Breastfeeding is good for mothers’ mental health – but those who struggle need support
Breastfeeding is good for mothers’ mental health – but those who struggle need support
In the words of the UNICEF Baby Friendly Initiative Call to Action: “It’s time to change the conversation.” We need to keep speaking out about breastfeeding and direct our trauma into action, until everyone who can plays their part in creating a supportive environment for new mothers.
Juno magazine: Why Breastfeeding Matters: it's more than just milk
Breastfeeding is good for mothers’ mental health – but those who struggle need support
Irish Times: Women who stop breastfeeding failed by system that doesn’t support them
Whilst formula milk may feed the baby, a woman’s expectations of her body do not go away because she can formula feed. A woman’s feelings that her body has let her down do not go away because she can formula feed. A woman’s desire to mother in the way she wants to do not go away because she can formula feed. And we must do more to recognise that.
Irish Times: Women who stop breastfeeding failed by system that doesn’t support them
Irish Times: Women who stop breastfeeding failed by system that doesn’t support them
Irish Times: Women who stop breastfeeding failed by system that doesn’t support them
Women who stop breastfeeding are failed by a system that fails to support them during breastfeeding and when they can’t, argues Prof Amy Brown.
What Do Women Lose if They Are Prevented From Meeting Their Breastfeeding Goals?
Irish Times: Women who stop breastfeeding failed by system that doesn’t support them
What Do Women Lose if They Are Prevented From Meeting Their Breastfeeding Goals?
This article explores the complex issue of breastfeeding and maternal mental health. Many women stop breastfeeding before they are ready, often leading to feelings of anxiety, guilt, and anger.
IHV: Supporting those who haven’t been able to breastfeed
Irish Times: Women who stop breastfeeding failed by system that doesn’t support them
What Do Women Lose if They Are Prevented From Meeting Their Breastfeeding Goals?
As part of #BreastfeedingCelebrationWeek, we are delighted to share a blog by Professor Amy Brown, Professor of Child Public Health at Swansea University, on why we must also focus on supporting those who haven’t been able to breastfeed.
Listen...
All in the Mind: Breastfeeding trauma
All in the Mind: Breastfeeding trauma
All in the Mind: Breastfeeding trauma
When breastfeeding goes wrong some women feel guilty that they have failed to do what should come naturally. But Professor Amy Brown from Swansea University says those with the most severe physical and emotional impact could be experiencing trauma, similar to the effects of a traumatic birth. We hear from Linzi Blakey who had problems with breastfeeding when she gave birth to her daughter and son and had to give up before she wanted to. A specialist therapist has helped her to realise that she did the best she could - despite a lack of the right kind of support when she was feeling vulnerable.
Midwives Cauldron podcast
Evolutionary parenting podcast
Midwives Cauldron podcast
In this episode we talk with the utterly wonderful Prof Amy Brown about why she doesn’t like sea lions, looking at breastfeeding from a biological perspective, women’s experiences of feeding their babies, how to navigate the internet as a birth worker and more!
The Next Feed Podcast
The Next Feed Podcast
The Next Feed Podcast
We look at how Amy came to be working in breastfeeding research, why she regularly speaks up for those experiencing breastfeeding grief and trauma, and how it doesn’t help anybody to be pitting formula against breastmilk. We also get into her very long list of frustrations on the lack of effort going into improving breastfeeding rates by those that have the power to about bring real change.
Copyright © 2026 Professor Amy Brown - All Rights Reserved.
